CMS CY 2027 Advance Notice Payment Accuracy Enforcement
- Ernie Ianace, CEO

- 6 days ago
- 3 min read
Why the CMS CY 2027 Advance Notice Matters More Than the Headline Rate
CMS released the CY 2027 Advance Notice with a headline number that immediately drew attention for the wrong reason. A net average payment increase of 0.09 percent is being described as flat, disappointing, or politically cautious. That framing understates what is actually happening.
The CMS CY 2027 Advance Notice is not primarily about rate setting. It is about enforcement through economics. CMS is signaling that future performance will be determined less by negotiated generosity and more by operational credibility. Payment accuracy, not payment expansion, is now the governing principle.
For Medicare Advantage plans, value-based care organizations, and clinical leaders responsible for execution, this marks a structural shift. CMS is treating the system as if it should already be capable of longitudinal documentation, encounter-based risk capture, and outcome-aligned care delivery. Whether that assumption is true will determine winners and losers over the next cycle.

Flat Rates as a Discipline Mechanism
The proposed effective growth rate of 4.97 percent is largely offset by risk model normalization and coding pattern adjustments, resulting in the 0.09 percent net increase. When estimated risk score trends are included, CMS projects an average revenue increase of approximately 2.54 percent.
This is not generosity. It is conditional tolerance.
CMS is making it clear that revenue growth will now come from accurate representation of patient complexity and consistent care delivery, not from aggressive retrospective optimization. Plans that have depended on post hoc documentation strategies will find less room to maneuver. Providers operating on thin margins will feel pressure to eliminate inefficiency rather than wait for relief.
In practical terms, the CMS CY 2027 Advance Notice turns inflation risk inward. Cost pressures are no longer an external justification for rate increases. They are an internal management problem.
Risk Adjustment Moves From Retrospective to Real
One of the most consequential proposals in the CMS CY 2027 Advance Notice is the exclusion of unlinked chart-review diagnoses from risk-score calculations beginning in 2027. Diagnoses not tied to a face-to-face encounter will no longer count.
This is a decisive move. It reframes risk adjustment as a reflection of lived care rather than reconstructed narratives.
CMS is explicitly devaluing retrospective chart sweeps that capture acuity without corresponding clinical action. The message is simple. If a condition did not surface in real care, it does not belong in the risk profile.
Combined with recalibrating the V28 model using 2023 diagnoses and 2024 expenditures, this change tightens the relationship between care delivery and revenue. Risk adjustment is no longer a separate optimization function. It is becoming inseparable from frontline workflows.
For organizations that already operate with strong clinical documentation at the point of care, this change will feel manageable. For those who rely on downstream correction, it will feel abrupt.
Quality Is Being Reweighted Toward Outcomes
While the Advance Notice governs payment math, the broader policy direction is reinforced by the momentum of the 2027 Proposed Rule. CMS is proposing removing 12 Star Ratings measures that are considered topped out, many of which are administrative or process-oriented.
This is an admission of maturity. CMS is acknowledging that compliance has plateaued and no longer differentiates performance.
At the same time, the introduction of a depression screening and follow-up measure in Part C and continued emphasis on patient experience indicate where accountability is moving. Clinical outcomes, behavioral health integration, and lived experience are replacing checkbox execution as performance signals.
The CMS CY 2027 Advance Notice should be read alongside these changes. Together, they point toward a system that expects fewer excuses and more proof.
What This Means for Leaders
The most important takeaway from the CMS CY 2027 Advance Notice is not the rate. It is the assumption embedded in the math.
CMS is acting as if longitudinal coordination already exists. As if encounter-based documentation is reliable. As if shared context flows across settings. In many organizations, that is aspirational rather than real.
The gap between assumption and reality will surface quietly. It will manifest as margin compression, unexplained variance, audit exposure, and operational strain long before it becomes formal enforcement.
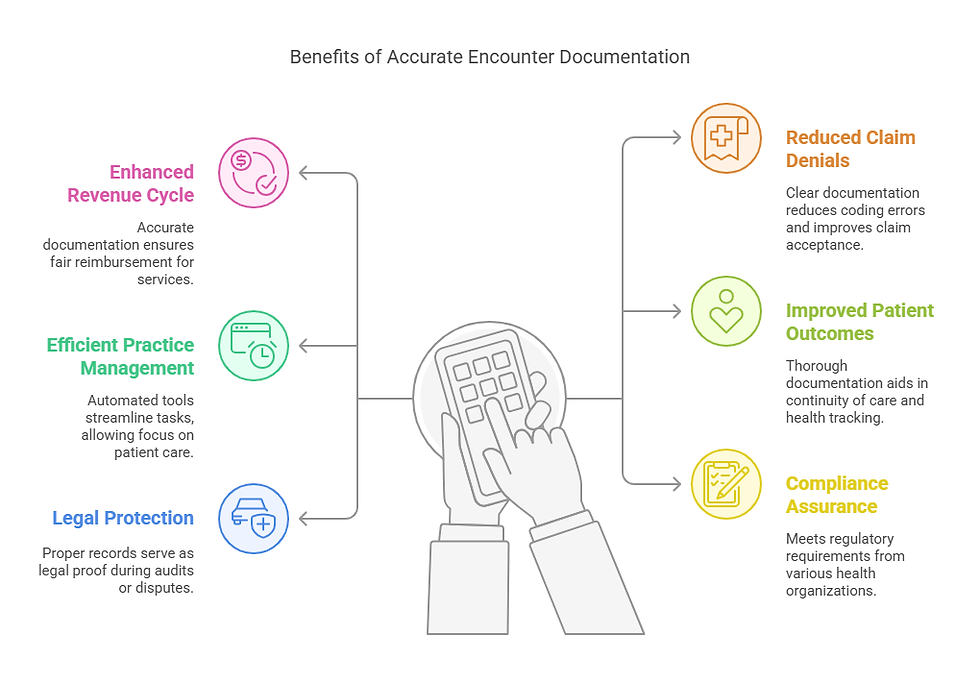
Organizations that invest in making care visible as it happens will be more resilient. Those that continue to treat documentation, quality, and risk as separate functions will struggle to reconcile them under a flatter payment environment.
The Signal Beneath the Numbers
CMS rarely needs to announce penalties when the economics already enforce behavior. The CMS CY 2027 Advance Notice is a clear example.
Payment accuracy is no longer a technical aspiration. It is the mechanism by which CMS is shaping the next phase of Medicare Advantage and value-based care.
The question for executives and clinical leaders is not whether this direction is fair. It is whether their organizations are ready to operate under it.


Comments